The role of blood thinners in preventing blood clots.
The Importance of Blood Thinners in Preventing Blood Clots
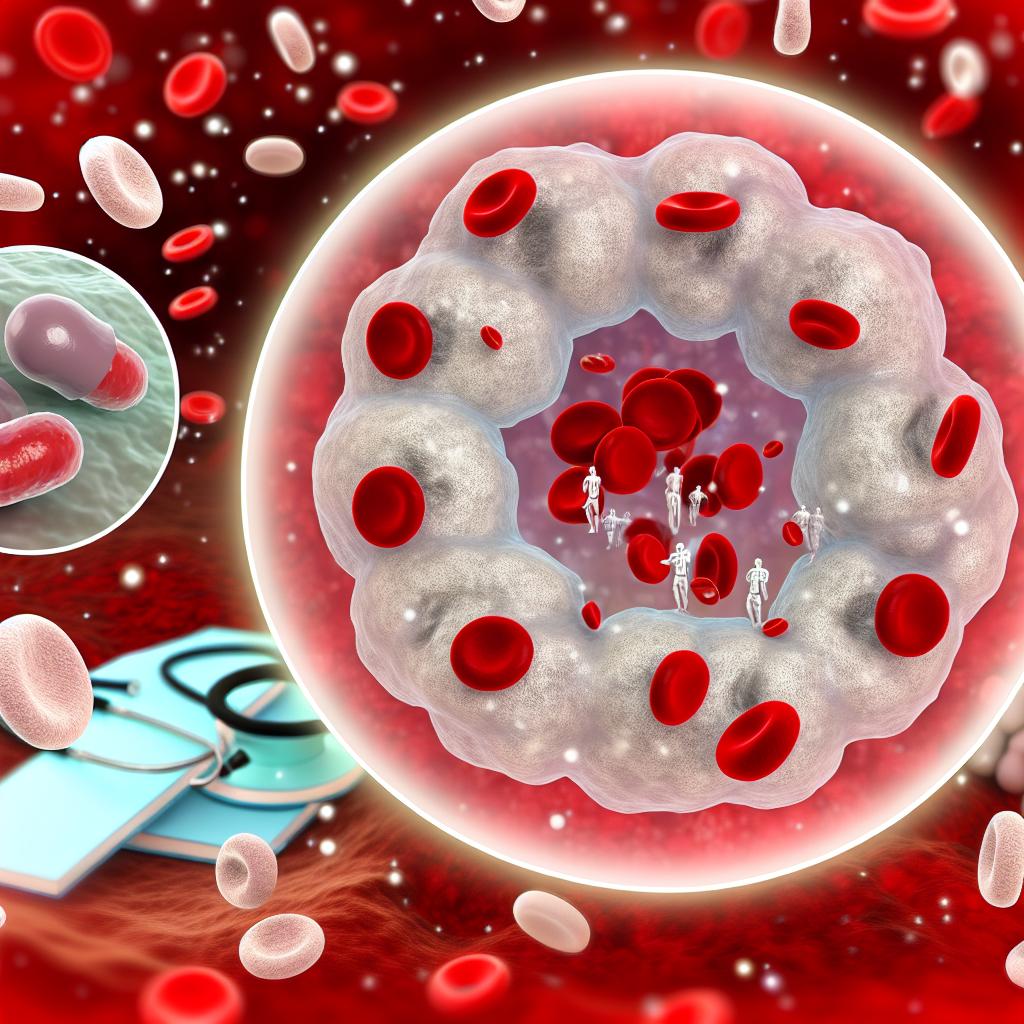
Blood clots pose a considerable health issue due to their potential to trigger severe conditions such as deep vein thrombosis (DVT), pulmonary embolism (PE), and an increased risk of stroke. The use of blood thinners, known in the medical community as anticoagulants, is a critical aspect of preventing these life-threatening occurrences. Understanding their function, application, and the necessary precautions is vital for patients and healthcare providers alike.
How Blood Thinners Work
Firstly, it is essential to clarify that the term “blood thinners” is somewhat misleading; these medications do not actually dilute the blood. Instead, they function by preventing the formation of new clots and by restricting the growth of existing ones. This important process is accomplished through the disruption of the blood’s clotting mechanism. Blood thinners target specific proteins that are integral to the clotting process. By doing so, they promote smoother blood flow and diminish the probability of clots obstructing veins and arteries, which can lead to severe complications.
Common Types of Blood Thinners
Blood thinners are categorized mainly into two groups: anticoagulants and antiplatelet drugs.
Anticoagulants include commonly prescribed medications such as warfarin and heparin, in addition to newer oral drugs like rivaroxaban and dabigatran. These drugs primarily disrupt elements of the coagulation cascade, a series of reactions crucial to blood clot formation.
On the other hand, antiplatelet drugs like aspirin and clopidogrel operate by preventing blood platelets from congregating. Since platelet aggregation is a preliminary step in clot formation, these drugs play a significant role in stalling the process before it progresses.
Indications for Blood Thinner Use
The prescription of blood thinners is generally contingent on specific risk factors or medical conditions that necessitate their use. Among the scenarios calling for these medications are:
– A previous history of blood clots or diagnosed clotting disorders that predispose an individual to recurrent clots
– Atrial fibrillation, which, due to irregular heart rhythms, can result in blood clots and significantly increase the risk of stroke
– Post-surgical contexts, notably following procedures like knee or hip replacements, where blood thinners may prevent post-operative clot formation
– Heart valve replacements, where long-term use of blood thinners is often recommended to reduce the risk of complications
In all these situations, the judicious use of blood thinners under professional supervision is crucial in reducing the risk of clot-related complications.
Potential Risks and Considerations
Despite their effectiveness, blood thinners are not without risks. A principal concern is the elevated risk of bleeding, which arises because the mechanism inhibiting clot formation also impedes the body’s ability to halt bleeding. Individuals on blood thinners must be vigilant about the following:
Regularly checking their blood levels is essential, especially for patients on anticoagulants like warfarin. This monitoring, often through a test known as the International Normalized Ratio (INR), helps in ensuring therapeutic levels are maintained without raising the risk of bleeding.
Careful engagement in physical activities, given the heightened risk of bruising or more severe injuries, is essential. Patients should be mindful of avoiding activities with a high risk of falls or collisions.
Communicating diligently with healthcare providers about any additional prescriptions or over-the-counter medications, including supplements, is vital. Many medicines can interact with blood thinners. For instance, non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can exacerbate bleeding risks when taken alongside anticoagulants.
Since lifestyle and dietary habits can influence clotting, it is imperative for individuals to strictly adhere to their healthcare provider’s guidance. Some dietary components, like Vitamin K found in leafy greens, can impact the effectiveness of certain blood thinners such as warfarin, requiring patients to maintain consistent dietary patterns.
Ongoing education and awareness for both patients and healthcare providers are vital for the effective use of blood thinners. Understanding the balance between the benefits and risks of anticoagulation therapy involves close partnership with healthcare professionals. For patients, this might include discussions about potential lifestyle adaptations that align with the therapeutic goals of using blood thinners.
For those seeking more extensive understanding or having specific queries, engaging with healthcare experts or reliable medical organizations can provide valuable insights and up-to-date information. This practice ensures that the use of blood thinners remains aligned with the latest evidence-based practices, thereby maximizing their efficacy in reducing the risk of clot-related health issues.
