The effects of antipsychotic medications on mental health.
Understanding Antipsychotic Medications
Antipsychotic medications, often referred to as neuroleptics, are primarily prescribed to manage psychotic symptoms in conditions such as schizophrenia and bipolar disorder. They function by altering the effects of neurotransmitters in the brain, which assists in reducing symptoms like hallucinations, delusions, and disorganized thinking.
How Antipsychotic Medications Work
Antipsychotics are categorized into two main groups: typical (or first-generation) and atypical (or second-generation) antipsychotics. Both types primarily work by blocking dopamine receptors, although atypical antipsychotics also affect other neurotransmitter systems, including serotonin.
Typical Antipsychotics
Typical antipsychotics, such as haloperidol and chlorpromazine, were developed in the 1950s. They tend to be effective in treating the positive symptoms of schizophrenia, which include hallucinations and delusions. However, they are often associated with side effects, notably extrapyramidal symptoms—these are drug-induced movement disorders that can have a significant impact on quality of life.
Extrapyramidal Symptoms
The primary concern when prescribing typical antipsychotics is the onset of extrapyramidal symptoms. These can include a range of movement disorders such as tremors, rigidity, and bradykinesia, which resembles the symptoms of Parkinson’s disease. Patients may also experience akathisia, characterized by a feeling of inner restlessness and a compelling need to be in constant motion. Additionally, dystonia, which involves involuntary muscle contractions leading to abnormal postures, can also occur. These side effects can be distressing for patients, often leading to issues with medication adherence.
Atypical Antipsychotics
Introduced in the 1990s, atypical antipsychotics include medications such as clozapine, risperidone, and olanzapine. These drugs tend to be more effective in addressing both positive and negative symptoms of schizophrenia, such as emotional withdrawal and apathy. Atypical antipsychotics are generally preferred due to a lower risk of causing extrapyramidal symptoms, though they are not without their own side effects.
Mechanisms Beyond Dopamine Blockade
While atypical antipsychotics do block dopamine receptors, their action is more nuanced. They also modulate serotonergic systems by blocking serotonin receptors, which is thought to mitigate some of the negative symptoms and cognitive deficits associated with schizophrenia. This feature makes atypical antipsychotics a more comprehensive treatment option, as they address a broader spectrum of symptoms compared to their typical counterparts.
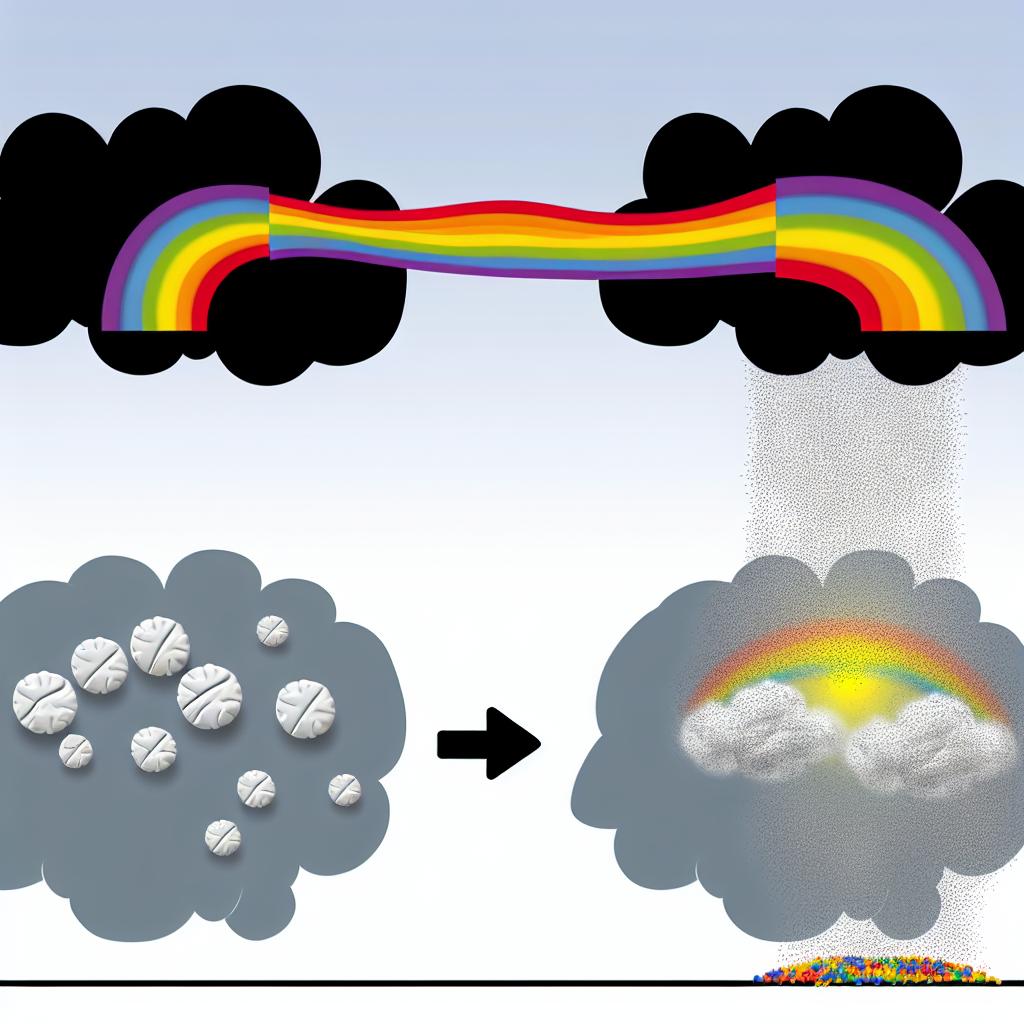
Benefits of Antipsychotic Medications
The primary advantage of antipsychotic medications lies in their ability to significantly reduce psychotic symptoms. For many individuals, these medications are vital in maintaining functionality and improving overall quality of life. By stabilizing mood and reducing the intensity of psychotic episodes, antipsychotics can allow individuals to engage more effectively in therapeutic and social activities.
Quality of Life Improvements
With the reduction of severe symptoms, individuals are often able to participate more fully in daily life. Improved symptom control can lead to enhanced social interactions, better job performance, and increased ability to accomplish personal goals. Antipsychotics can play a crucial role in restoring independence and contributing to a sense of normalcy for those affected by severe mental illnesses.
The Role of Antipsychotics in Preventing Relapse
Consistent use of antipsychotic medications is known to decrease the likelihood of relapse. This is particularly important because each psychotic episode can lead to cumulative cognitive and functional decline. By preventing these episodes, antipsychotics help maintain long-term health and stability, which in turn supports recovery-oriented goals and aids in reducing the need for hospitalization.
Potential Side Effects and Risks
While antipsychotics are effective, they are also associated with a variety of side effects. Understanding these potential risks is crucial for both patients and healthcare providers.
Common Side Effects
Common side effects from antipsychotics may include drowsiness, weight gain, and increased risk of diabetes. Atypical antipsychotics, in particular, have been implicated in metabolic syndromes, which require monitoring and lifestyle adjustments.
Metabolic Side Effects
Weight gain is a significant concern with atypical antipsychotics due to its association with metabolic syndrome. This condition includes a cluster of symptoms like increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels. These factors can elevate the risk of heart disease, stroke, and type 2 diabetes, underscoring the necessity for diligent monitoring of patients on these medications.
Long-term Risks
Prolonged use of antipsychotic medications can lead to tardive dyskinesia, a condition marked by involuntary muscle movements, usually in the face and tongue. Additionally, there is a need for regular assessment of metabolic health parameters due to the potential for developing cardiovascular issues.
Tardive Dyskinesia: An Ongoing Concern
Tardive dyskinesia is a serious and often irreversible effect that can arise after long-term or high-dosage antipsychotic use. The involuntary movements associated with this condition can significantly hamper a patient’s quality of life. Though atypical antipsychotics pose a reduced risk compared to typical antipsychotics, the possibility remains, emphasizing the need for routine follow-up and evaluation.
Importance of Monitoring
Regular physical check-ups, including metabolic assessments and movement disorder evaluations, are essential components of a comprehensive care plan for individuals on long-term antipsychotic therapy. Adjustments in lifestyle, diet, and exercise may be recommended to counteract these effects, alongside regular consultations with healthcare providers to tailor treatment strategies.
Conclusion
Balancing the therapeutic benefits of antipsychotic medications against their side effects is an ongoing challenge in psychiatric care. Individual treatment plans should be regularly reviewed and adjusted by healthcare providers to optimize outcomes. For further reading on managing the effects of antipsychotic medications, consider exploring research articles or guidelines provided by mental health organizations and professional groups.
Future Directions in Antipsychotic Treatment
As the field of psychiatry continues to evolve, there is ongoing research into new pharmaceutical approaches that might offer improved efficacy and tolerability compared to current options. Developing medications that specifically target underlying pathologies with fewer side effects remains a key goal. Advances in genetic and biomarker research may lead to more personalized approaches, tailoring antipsychotic treatment to the individual’s unique biological profile.
The Role of Patient Education and Involvement
Empowering patients with knowledge about their treatment options, potential side effects, and the importance of adherence can foster better therapeutic alliances and outcomes. By collaborating closely with healthcare providers and engaging in shared decision-making, patients can play a proactive role in managing their mental health conditions.
In summary, while antipsychotic medications are an essential component of treatment for psychotic disorders, it is crucial to weigh their benefits against potential risks. Continuous monitoring and personalized care strategies remain fundamental to maximizing their effectiveness and minimizing adverse effects.
