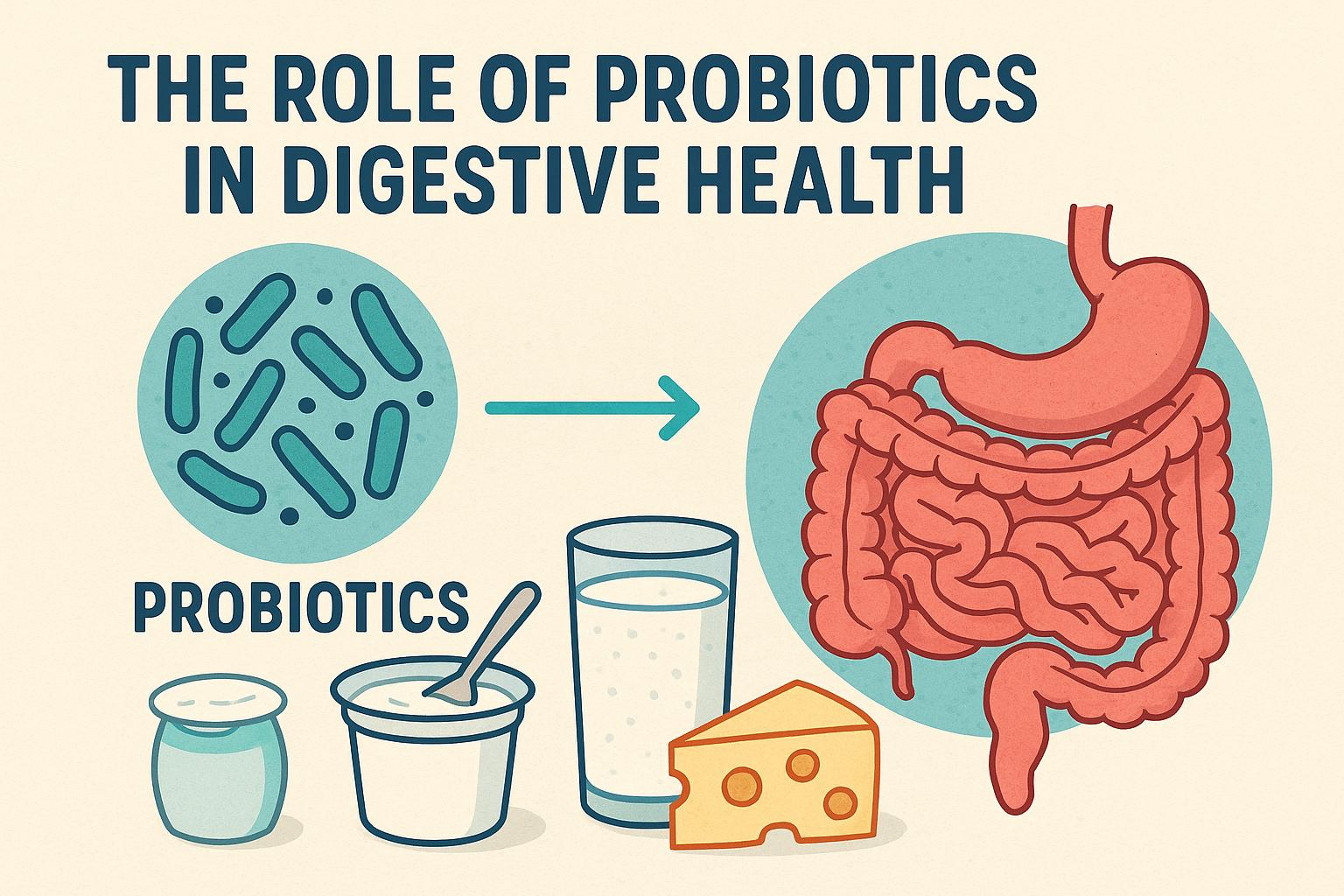
The role of probiotics in digestive health.
The Importance of Gut Health
The human digestive system is crucial to maintaining overall health, going beyond its primary role of digesting food to have significant impacts on the immune system and mood regulation. Recent scientific advancements have further underscored the critical importance of sustaining a balanced gut microbiota—the term used to describe the diverse community of microorganisms residing within the gastrointestinal tract. This community, comprising bacteria, viruses, fungi, and other microorganisms, plays a pivotal role not just in digestion but across various aspects of health.
Understanding Probiotics
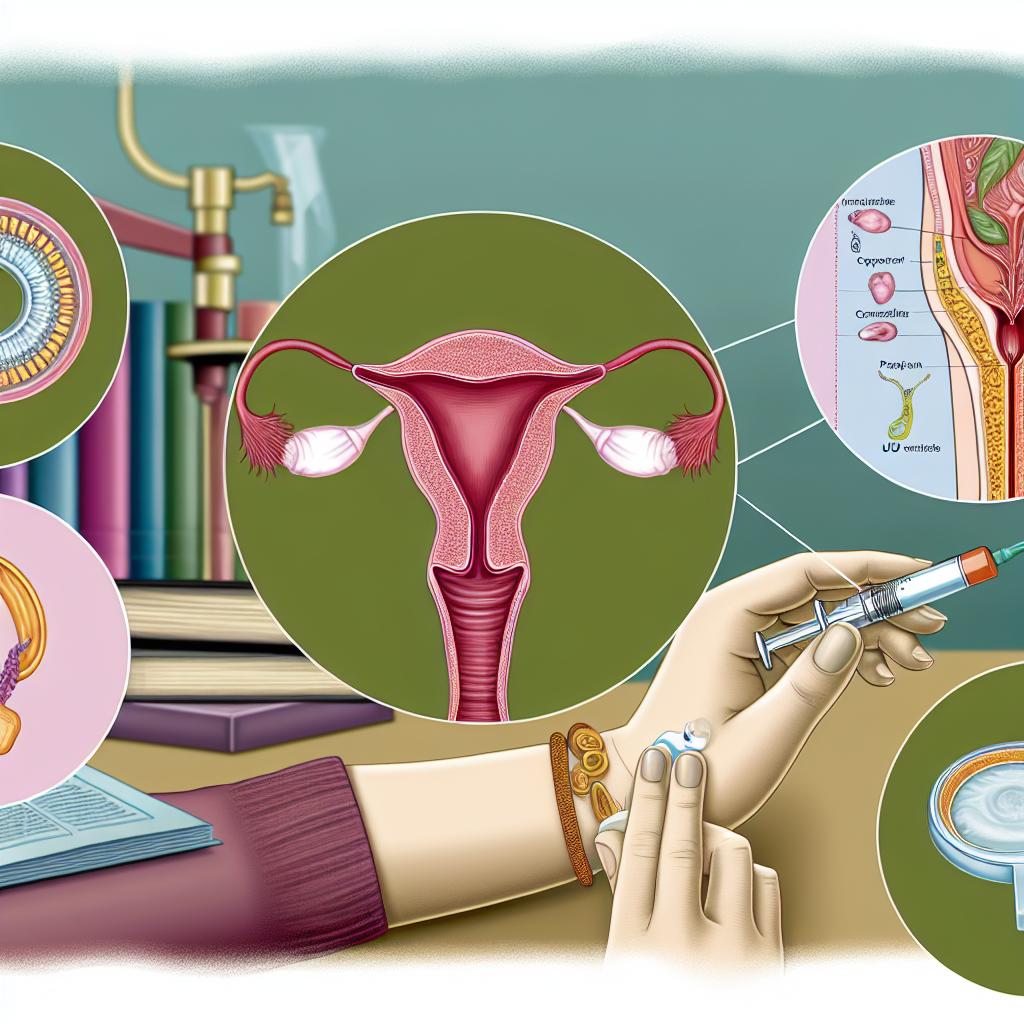
Probiotics, often referred to as “good” or “friendly” bacteria, are live microorganisms that provide a health benefit to the host when consumed in adequate amounts. They are primarily recognized for their contribution to supporting and enhancing digestive health. Typically, probiotics can be located in fermented foods, such as yogurt, kefir, and sauerkraut, as well as within dietary supplements designed to provide specific strains.
How Probiotics Work
The primary function of probiotics is to help maintain the delicate balance of the gut microbiome, which is susceptible to disruption by various factors including illness, the use of antibiotics, or even a poor diet. By integrating probiotics into one’s daily dietary regimen, it is possible to restore this balance and thus positively influence not only digestion but also the overall function of the immune system.
Gut Microbiota Diversity plays an essential role in this context. A microbiota with a high diversity of microorganisms is generally considered beneficial for optimal health, aiding in the breakdown of complex carbohydrates, synthesizing essential vitamins like B12 and K, and offering protections against harmful pathogens.
Health Benefits of Probiotics
Digestive Health: Probiotics are commonly recommended for the management of various digestive disorders including irritable bowel syndrome (IBS), diarrhea, and constipation. By regulating bowel movements and minimizing symptoms such as bloating, probiotics can contribute to enhanced digestive comfort.
Immune Function: A well-maintained gut microbiome can significantly bolster the body’s immune responses. Probiotics promote the production of antibodies and enhance the activities of specialized cells that defend the body against infections.
Mental Health: Emerging research has identified a fascinating link between gut health and mental well-being, a connection frequently termed the gut-brain axis. Probiotics may help in alleviating symptoms associated with mental health conditions such as anxiety, depression, and stress by modulating the bacteria present in the gut.
Choosing the Right Probiotic
Given the diversity among probiotics, selecting the most appropriate one can be complex. It is imperative to consider the specific strains contained and their documented health benefits. Each strain may serve distinct functions, and hence consulting with a healthcare provider can prove advantageous for tailoring choices to individual health needs.
Additionally, verifying that the probiotic products chosen contain live and viable bacteria is crucial, as certain probiotics may lose effectiveness if improperly stored or handled. Packaging that indicates a high number of CFUs (colony-forming units) can provide guidance on the probable efficacy of the product.
Conclusion
Incorporating probiotics into the daily diet holds numerous potential benefits for digestive health and beyond. By promoting a balanced gut microbiota, probiotics can enhance nutrient absorption, improve immune system performance, and support mental well-being. Continuous research will no doubt further expand the understanding of these beneficial microorganisms, reinforcing their importance in the maintenance and promotion of overall human health.