How birth control methods other than pills work.
Understanding Birth Control Methods Beyond the Pill
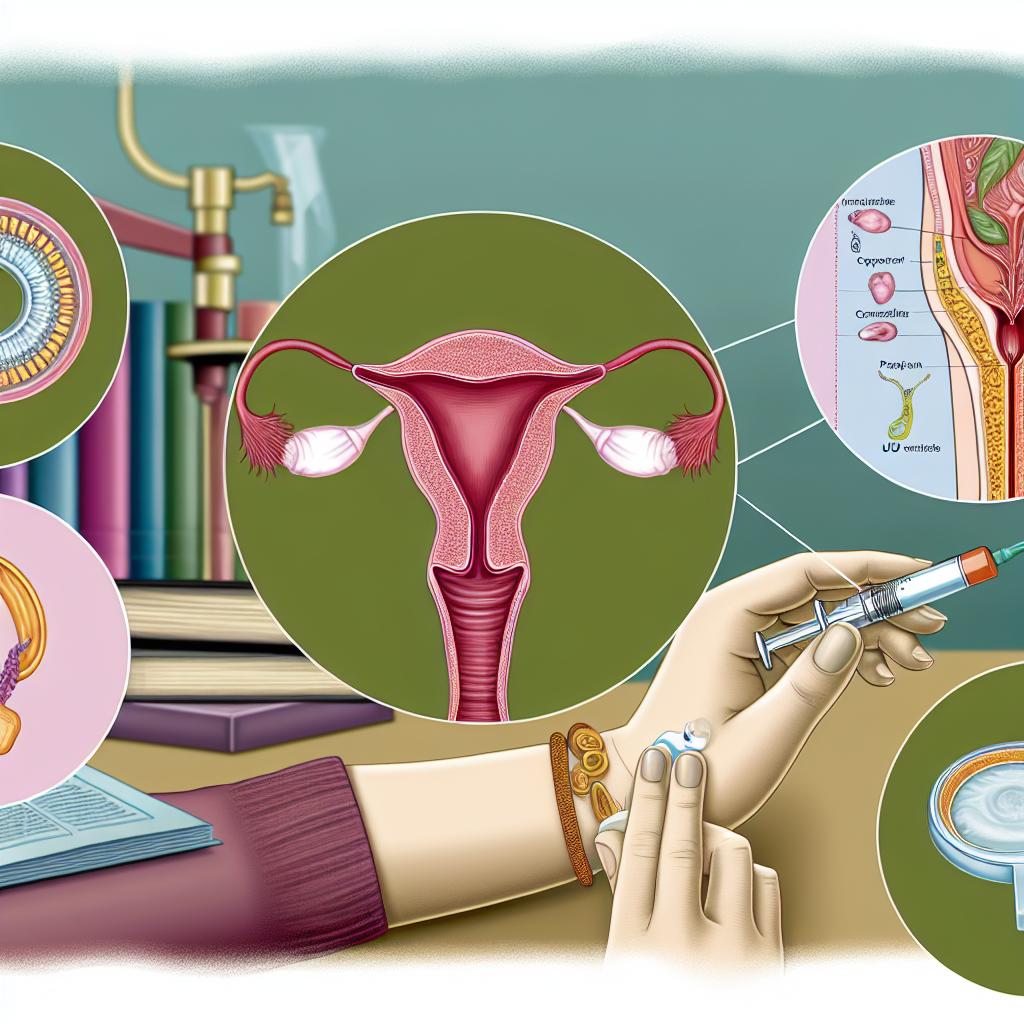
When many individuals consider birth control, their thoughts often turn to the most familiar option: oral contraceptives, also known as “the pill.” However, a wide array of alternatives exist; they are just as effective, if not more so, and serve different health and lifestyle needs. These options include methods that do not require daily attention, and a brief overview of such methods is outlined below to support informed decision-making regarding reproductive health.
Implants
An implant is a notable long-term birth control solution. This small, flexible rod, usually no longer than a matchstick, is inserted just under the skin of the upper arm by a trained healthcare provider. Once in place, the implant releases a steady dose of progestin, a hormone that prevents the ovaries from releasing eggs, also known as ovulation. Additionally, progestin increases the thickness of the cervical mucus, providing an extra barrier to sperm entering the uterus. What makes implants particularly appealing is their long-term effectiveness, typically lasting up to three years. This attributes to them being a reliable option for those looking for a low-maintenance and highly effective form of contraception. It’s critical for individuals considering an implant to consult with their healthcare provider to understand potential side effects and address any questions they might have.
Intrauterine Devices (IUDs)
Intrauterine devices, commonly referred to as IUDs, come in two primary types, each working through distinct mechanisms to prevent pregnancy.
Hormonal IUDs function similarly to implants. They release progestin directly into the uterus. The hormone thickens the cervical mucus, which is instrumental in preventing sperm from reaching the egg. In some cases, hormonal IUDs may also suppress ovulation. The lifespan of hormonal IUDs ranges from three to seven years, varying according to the device’s brand and design. Their local release of hormones means many users experience fewer systemic side effects compared to oral contraceptives.
Copper IUDs offer a hormone-free alternative. The copper material slowly releases ions that create a toxic environment for sperm, thereby inhibiting fertilization. Once inserted, copper IUDs can remain effective and in place for up to ten years, marking them as one of the most enduring birth control options available. Because they don’t rely on hormones, copper IUDs might be preferred by those who want to avoid hormonal side effects altogether.
In both types, it is essential for the device to be properly placed by a healthcare provider. Users should have follow-up exams to ensure the IUD remains in the correct position.
Injectable Contraceptives
Injectable contraceptives, or “the shot,” comprise another alternative in the spectrum of birth control solutions. This method involves a healthcare professional administering a shot, most commonly every 12 weeks. The injection usually contains the hormone progestin, serving the dual function of suppressing ovulation and thickening cervical mucus. It’s effective but requires adherence to a strict schedule; missing an appointment can compromise its effectiveness. For individuals who prefer a less frequent regimen than daily pills or weekly patches, and who may not be interested in long-term implantable devices, injectables provide a nice middle ground. As with any hormonal method, potential side effects should be discussed with a healthcare provider.
Contraceptive Patches
The contraceptive patch represents an intermediary level of commitment and maintenance. It’s a small, sticker-like patch applied to the skin that delivers a combination of hormones—estrogen and progestin—directly into the bloodstream. The patch is worn on the skin for one week at a time over a three-week period, followed by a patch-free week to allow for a withdrawal bleed akin to a menstrual period. This method replicates the primary function of the pill, stopping ovulation and thickening cervical mucus, but offers ease of use similar to that of the monthly shot for those who might struggle with daily routines. Users should be cognizant of potential skin reactions at the application site and the importance of consistent usage schedules.
Vaginal Rings
Vaginal rings offer another choice for those desiring a hormonally driven method with less daily upkeep. A flexible ring is inserted into the vagina, where it remains for three weeks, releasing a steady dose of estrogen and progestin. The ring is removed during the fourth week to permit a withdrawal bleed, after which a new ring is placed. User discretion and education play a role in the success of this method, as it involves routine self-placement and timely changes every month.
Barrier Methods
Barrier methods differ significantly from hormone-based approaches as they physically impede sperm from reaching the egg. They vary widely in form and application.
Male and female condoms are the most recognized barrier methods. Male condoms fit over the penis, while female condoms line the vaginal interior. Both provide effective prevention against pregnancies and sexually transmitted infections (STIs) by acting as a physical barrier.
Spermicides
Spermicides are chemical products that immobilize or kill sperm, inserted into the vagina before intercourse. Sometimes used in conjunction with barrier methods, they can further increase prevention efficacy. While effective, it is essential to adhere closely to the instructions for use to maximize their viability as a contraceptive choice.
These methods present not only a wide array of choices but also a spectrum of benefits and considerations that each individual must weigh alongside their personal health circumstances and lifestyle preferences. Consulting healthcare professionals and accessing reputable sources, such as Planned Parenthood, offer further insight and personalized recommendations, ensuring that each person can choose the best method suited to their needs.
