The uses and side effects of mood stabilizers.
Understanding Mood Stabilizers
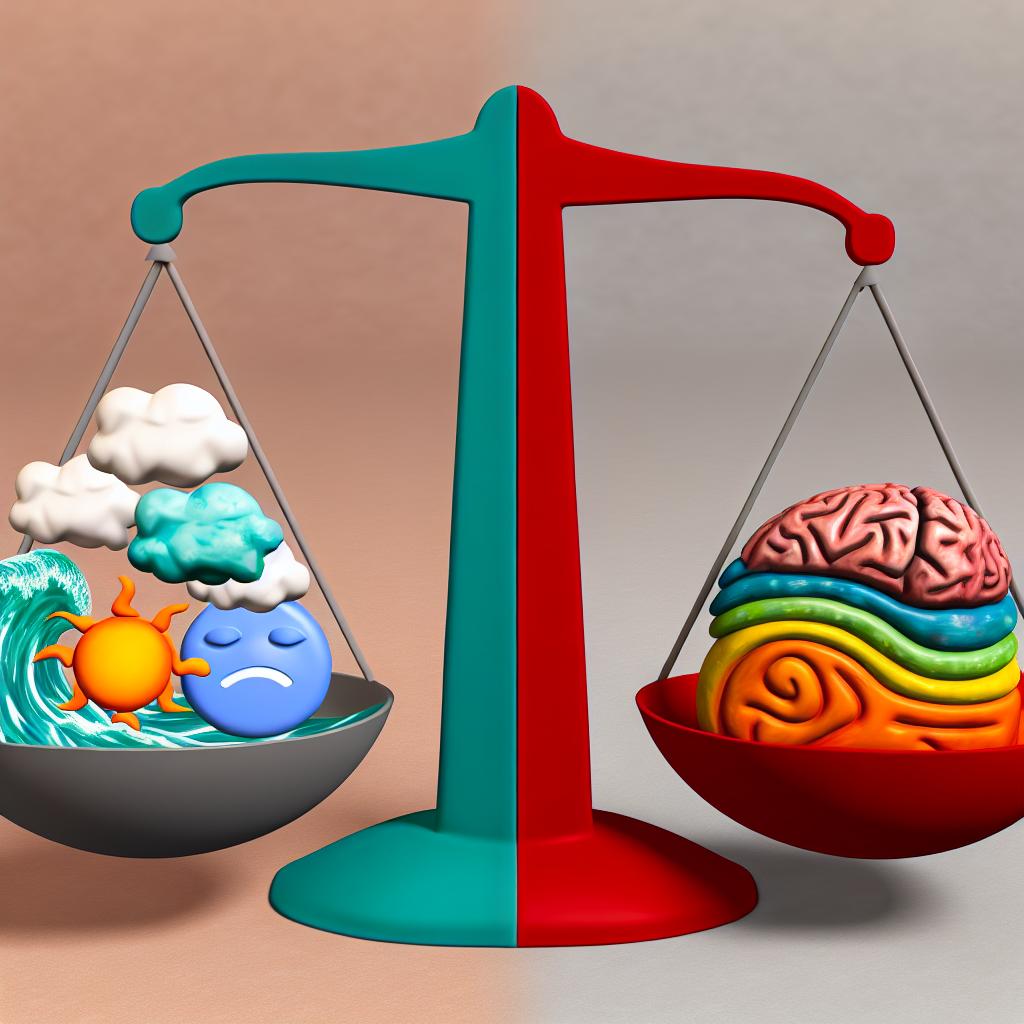
Mood stabilizers are a class of medications primarily used to treat mood disorders characterized by extreme mood swings, such as bipolar disorder. They are essential in stabilizing mood by preventing episodes of mania, hypomania, and depression. Mood stabilizers can be fundamental in maintaining a patient’s ability to function and ensuring a higher quality of life.
Common Uses of Mood Stabilizers
Mood stabilizers are mainly prescribed for individuals diagnosed with bipolar disorder, where they help in minimizing the intensity and frequency of mood episodes. They can also be beneficial for some individuals with schizoaffective disorder, depression with mood instability, or certain neurological conditions presenting mood disturbances.
These medications are effective in managing the symptoms by balancing certain chemicals in the brain. This can lead to a significant decrease in manic or depressive episodes, allowing individuals to lead more stable lives.
Types of Mood Stabilizers
Mood stabilizers come in various forms to address different aspects of mood stabilization, each providing a unique approach to managing symptoms.
Lithium: As one of the oldest and most traditional mood stabilizers, lithium has long been heralded for its efficacy in controlling manic episodes and reducing the risk of suicide. Its use is based on extensive research and clinical data showcasing its ability to offer long-term management of mood symptoms.
Anticonvulsants: Medications like valproate and lamotrigine, originally designed for seizure control, have demonstrated significant mood-stabilizing properties. They are particularly useful for individuals who may not fully respond to lithium. Anticonvulsants work by decreasing abnormal electrical activity in the brain, thus stabilizing mood.
Atypical Antipsychotics: Drugs such as olanzapine and quetiapine, while primarily antipsychotic in nature, possess mood-stabilizing benefits. They are often used in conjunction with other treatments to enhance mood stabilization, and their use depends on the individual’s unique symptom profile.
Potential Side Effects of Mood Stabilizers
The side effects of mood stabilizers can vary based on the specific medication and the individual’s physiological response. While they can be highly effective in managing mood disorders, understanding these side effects is crucial for both patients and healthcare providers to manage treatment plans effectively.
Common Side Effects
Patients may experience a variety of side effects, which can impact adherence to the treatment. Understanding these potential risks helps in making informed decisions about using mood stabilizers.
Lithium: Potential side effects for lithium include weight gain, increased thirst, frequent urination, hand tremors, and possible thyroid or kidney issues. Long-term use requires careful monitoring of renal and thyroid function due to the potential cumulative effects.
Valproate: Common side effects may encompass weight gain, hair thinning, drowsiness, and potential liver damage with prolonged use. Regular liver function tests are essential to prevent hepatic complications.
Lamotrigine: Users might face the risk of severe skin rashes, known as Stevens-Johnson syndrome, along with headaches and dizziness. Gradual dose increases are vital to minimize these risks.
Monitoring and Management
Monitoring mood stabilizer therapy is essential to balance effectiveness and side effect management. It involves a comprehensive approach, including laboratory testing and dose adjustments.
Regular blood tests often accompany the use of mood stabilizers to ensure therapeutic drug levels, especially for lithium and valproate. These tests help prevent toxicity and optimize the dosage to maintain sufficient symptom control without undue side effects.
Dose adjustments might be necessary to strike a balance between efficacy and tolerability. Healthcare providers often make changes based on both clinical assessment and blood test results.
Communication with Healthcare Providers
Open communication between patients and their healthcare providers is essential. Establishing a rapport encourages patients to share their experiences, report any troubling side effects promptly, and work with their healthcare providers to find the most suitable treatment plan.
Finding the most effective mood stabilizer or combination of medications can take time. It requires patience and collaboration between the patient and healthcare provider to identify the treatment plan that provides maximum symptom control with minimal side effects.
Healthcare providers should offer clear guidance on managing side effects and advise on the importance of adhering to prescribed treatment regimens. Patients should feel empowered to voice concerns, thereby contributing to the formulation of a tailored treatment approach.
Resources and Further Reading
For more in-depth information on mood stabilizers, consider exploring reputable medical resources such as those provided by healthcare institutions or research organizations. Engaging with current research can provide insights into new developments in mood stabilization therapies.
Valid online resources can offer further insights into managing and understanding these essential medications. Accessing comprehensive guides and peer-reviewed articles can enhance understanding and aid in informed decision-making.
As the understanding of mood disorders and mood stabilizers continues to evolve, staying informed about the latest research can benefit both patients and healthcare providers in optimizing treatment strategies for mood regulation.